| Item | Price | Qty | Total | |
|---|---|---|---|---|
 Loading Cart...
Loading Cart...Why Are We Still Debating Platelet-Rich Plasma?

In the 2000s, when Platelet-Rich Plasma first started shifting its role from being a healing assistant in cardiac and orthodontic surgeries to the more leading role of healing bone grafts and joint tissues, many leading physicians claimed that the practitioners were putting profiteering before truth and science. They even said it was outright theft to charge $300 for an injection that, according to them, had an efficacy no less than placebo. That was in 2009 and the confusion back then was justifiable.
Fast forward 7 years later, in 2016, and we had the first FDA-Sanctioned, Randomized, Double-blind, Placebo-controlled Clinical Trial on Platelet-Rich Plasma for Knee Osteoarthritis which showed that PRP improved the outcome by 78% compared to 7% for placebo.
This was also confirmed by two Chinese major review studies this year, both Meta-analysis of Randomized Controlled Trials of Platelet-Rich Plasma for Knee Osteoarthritis – first one here and the second one here.
Yet, we still see physicians here in the US – orthopedists and rheumatologists, among them – who don’t even bother to try it once on their patients!
What’s going on?

The Hidden Factor That’s Holding PRP Back
Platelet-Rich Plasma, as we know, contains 7X-9X concentration of platelets in a serum with a balanced ratio of plasma, leukocytes and RBC. This special mixture helps supply growth factors and other proteins that tissues can use to recruit stem cells and heal itself. This process is pretty straight-forward. Yet, we know for a fact that there are some physicians who fail to see results with Platelet-Rich Plasma, including some clinical studies performed by veterans.
Are they missing something?
We suspect it has got to do with the second part to PRP’s healing mechanism. It’s right application.
It can be summed up in the following two questions.
- Precisely which tissue are you delivering the PRP to?
- How are you making sure that the PRP is used by the tissues and not wasted?
This is where the science of Interventional Orthopedics come into play.
The Science Behind Interventional Orthopedics
On the outside, interventional orthopedics look very simple. You identify the area which needs healing, and then administer Platelet-Rich Plasma (or stem cells for that matter) to that particular area and wait for it to heal. Thinking that its this simple screws up the process for physicians who’re merely trying their luck with PRP. Because, the bulk of the Platelet-Rich Plasma treatment – the actual work that the physicians need to do – has to do with the following.
- Identifying the exact group of tissues that are broken or degenerated (Accurate Localization),
- Creating lesions in the damaged tissue, and
- Delivering Platelet-Rich Plasma precisely at that location.
These advanced injections are much more effective and requires a different level of expertise.
For example, typical injections in the knee can only deliver the Platelet-Rich Plasma serum to the synovial fluid, synovial membrane and articular cartilage. The advanced injections like intraosseous infiltrations can deliver the PRP serum to the subchondral bone and the deep layers of cartilage that are affected by Osteoarthritis.
These kind of advanced injections require the use of fluoroscopic guidance for proper administration as well as proper training on the physician’s side.
Here’s one study that explains why accurate localization is linked with an improved clinical outcome – Study of intra-articular infiltrations with intra-osseous injections of Platelet-Rich Plasma.
The thing is, not all physicians are trained to do it. The scope of these advanced injections are vast and warrant extensive training and expertise.

To continue with the example of the knee, most physicians are proficient only in the superomedial or anteromedial/anterolateral injections to the knee. However, advanced Platelet-Rich Plasma injections can deliver the PRP to precise locations like…
- Medial collateral ligament (MCL)
- Posterior cruciate ligament (PCL)
- Anterior cruciate ligament (ACL)
- Lateral collateral ligament (LCL)
- Patellar ligament (PL)
- Quadriceps tendon
- Patellar tendon
- Medial meniscus
- Anteromedial joint line (AMJL)
- Medial midpatellar (MMP)
- Superomedial patellar (SMP)
- Anterolateral joint line (ALJL)
- Lateral midpatellar (LMP)
- Superolateral patellar (SLP)
- Lateral suprapatellar bursa (LSB)
- Infrapatellar (IFP)
- Lateral meniscus
- Subchondral bone
- Femur bone
Most physicians, instead of getting highly proficient in identifying and administering precise PRP injections, they get concerned over the relative lack of protocols for PRP Injections. They get carried away by details like the frequency of the injection, the leukocyte levels, and red blood cells, when the fact is… as long as you get the platelet concentration right (5X-9X baseline), the therapeutic effects are guaranteed. The frequency and the presence of Leukocytes are minor factors that have little to no impact on the outcome.
The most important factor is physician training for advanced injections under Ultrasound or Fluoroscopy.
If It Works For Knee Osteoarthritis, It Probably Works For Other Degenerative Diseases
There is another concern among some physician who claim that there’s no evidence for the particular condition that they’re treating. For example, let’s say they’re treating Spinal muscular atrophy in a patient and see that there has been no study that proves Platelet-Rich Plasma is a good candidate.
Does that mean it won’t work? Absolutely no.
It just means no one has ever studied it in detail. The working mechanism behind Platelet-Rich Plasma is so universal that if it works for the knees, it will work for the spine and other similar areas of the body as well. In fact, there is almost no part of the body that is not currently known to have a therapeutic effect upon application of Platelet-Rich Plasma – nerves, joints, muscles, skin, hair, and even the eyes are treated by PRP.
By the way, if you’re wondering if there really is a study on Platelet-Rich Plasma for Spinal Muscular Atrophy, here is one from Egyptian researchers.
Does Age Play A Role?
We’ve noticed that age does not have a correlation with the effectiveness of Platelet-Rich Plasma injections. It works just the same for the young and old.
However, the one thing that do have a correlation is the degree to which the disease has advanced.
The more advanced the disease, the less likely that Platelet-Rich Plasma can reverse its course. That is the reason why we recommend physicians treat Platelet-Rich Plasma as a first-line treatment for all possible conditions. It has already shown to be much more effective than both Cortisone and Hyaluronic Acid injections.

Education in Advanced regenerative-medicine injections
So, back to the single biggest needle-mover when it comes to Platelet-Rich Plasma injections: ACCURATE LOCALIZATION. This means the physicians must undergo advanced training for this type of injections.
And there are not many options available until recently.

Thankfully, we now have the Interventional Orthopedics Foundation (IOF) foundation – the first non-profit in the US dedicated to providing training for core injection skills. According to IOF, only 1% of the physicians in the US are trained to do these advanced injections. And chances are you may not have been trained.
With IOF, you can get trained for that in a real medical setting with skilled instructors and support staff.
According to the IOF website, they can train you on:
- Injections for the healing of bone, tendon, ligaments, muscle or cartilage.
- Accurate localization of these injections on damaged structures using image guidance.
- New tools that facilitate percutaneous tissue manipulation.
This is a wonderful non-profit education initiative by Christopher J. Centeno, MD, Gregory Lutz, MD, Don Buford, MD and Richard D. Striano D.C., RMSK, all leading players in the regenerative medicine field.
Here’s a video you can watch to learn about IOF foundation.
And check out the IOF membership information here.
One last thing…
Platelet-Rich Plasma Standardization
As a Platelet-Rich Plasma practitioner, you’ll be out on the leading-edge. You’ll discover things that others may not be aware of. And you’ll have the opportunity to publish your findings. That’s when you’ll think of a standardization. By then, it’s too late. You’ve already performed a lot of injections and your data in unstandardized.
To avoid this, consider using a standard for the preparation of Platelet-Rich Plasma.
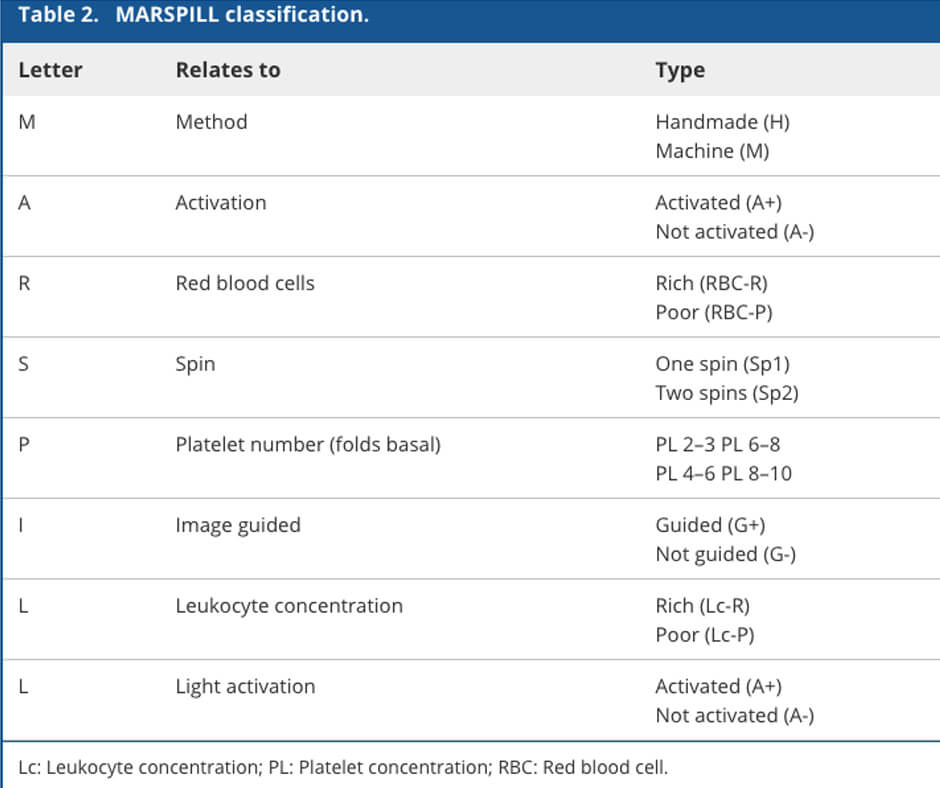
We suggest using the latest MARSPILL classification for Platelet-Rich Plasma developed jointly by Brazilian and US researchers.
The lack of standardization is the main culprit when it comes to debates over the efficacy of Platelet-Rich Plasma. We would love to see more and more researchers and everyday practitioners accepting a common standardized classification system for PRP.
Here’s the chart for the MARSPILL classification.
And you may also want to check out the DRPRP Kit for the most ideal concentration of Platelet-Rich Plasma.



